Vascular care
1st Apr 2024
Peripheral Arterial Disease: Risks, Occupations and Complications of Untreated PAD
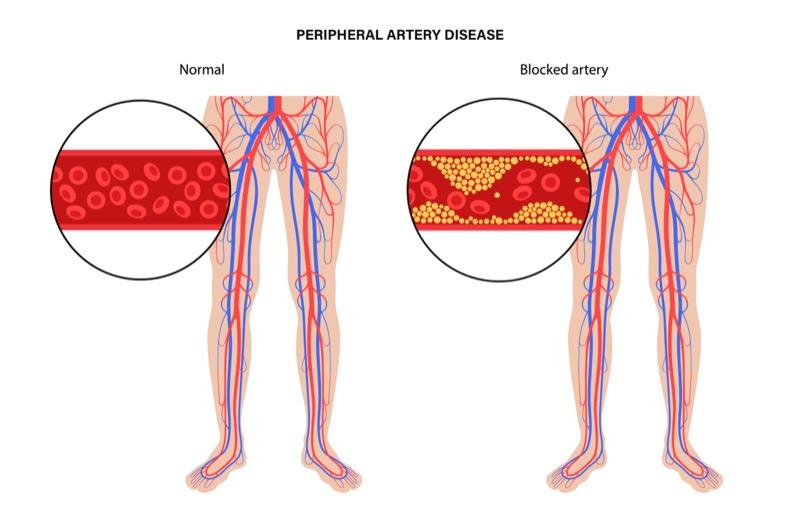
Understanding Peripheral Arterial Disease
Peripheral arterial disease (PAD) is a progressive condition characterized by the narrowing or blockage of the arteries that carry oxygenated blood from the heart to the limbs, primarily the legs. This reduced blood flow can lead to various symptoms and complications, making PAD a significant health concern globally. Our vascular care specialists provide comprehensive treatment options for this condition.
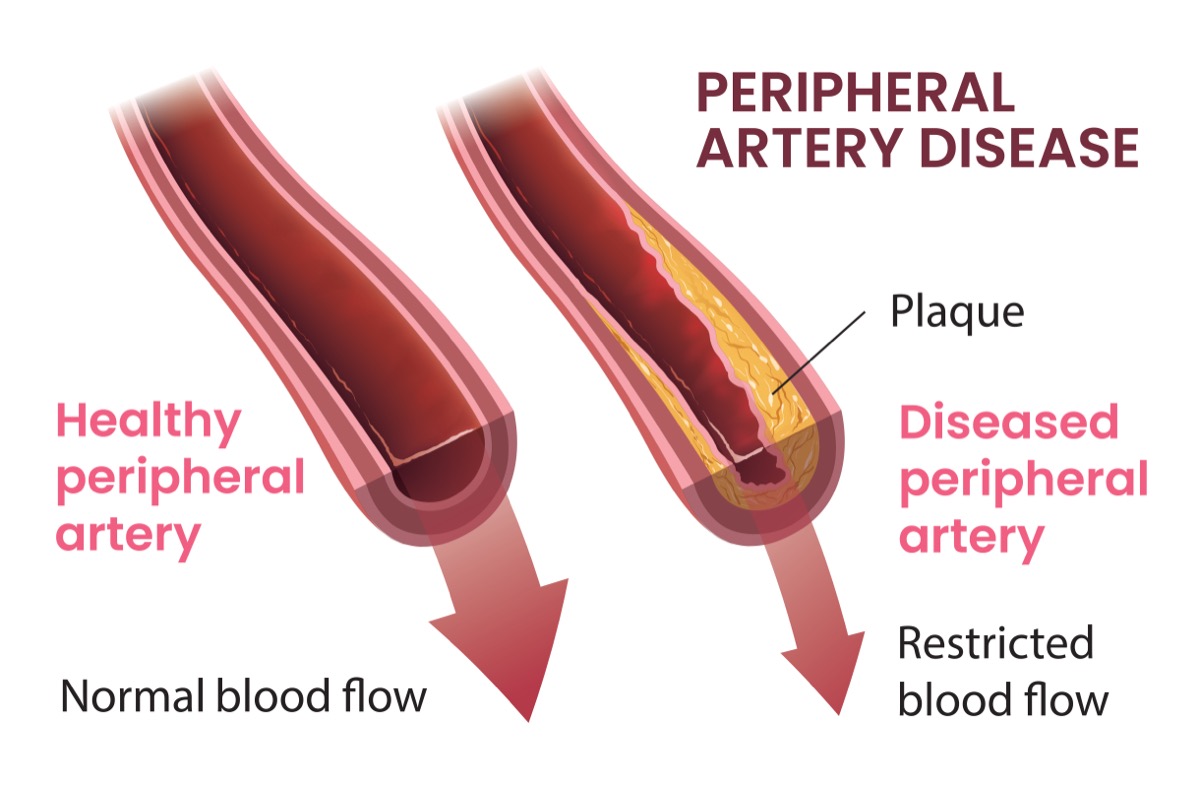
The primary cause of PAD is atherosclerosis, a buildup of fatty deposits (plaque) within the arterial walls, gradually narrowing the vessels and restricting blood flow. While PAD can affect arteries throughout the body, it most commonly impacts the legs and feet.
Causes and Risk Factors
Atherosclerosis, the underlying cause of PAD, is influenced by several modifiable and non-modifiable risk factors:
- Smoking: Tobacco use is a significant risk factor for PAD, as it damages the arteries and promotes plaque buildup.
- Diabetes: Individuals with diabetes are at an increased risk of developing PAD due to the damaging effects of high blood sugar levels on the arteries.
- High Blood Pressure: Uncontrolled hypertension can damage the arterial walls, leading to the formation of plaque.
- High Cholesterol: Elevated levels of low-density lipoprotein (LDL) cholesterol can contribute to plaque buildup in the arteries.
- Obesity: Being overweight or obese increases the risk of PAD, as it can lead to other risk factors like diabetes and high blood pressure.
- Age: The risk of PAD increases with age, as the arteries naturally become stiffer and more susceptible to plaque buildup over time.
- Family History: Having a family history of PAD, heart disease, or stroke can increase an individual’s risk of developing the condition.
- Occupational Factors: Certain professions that involve prolonged sitting, standing, or exposure to environmental pollutants may increase the risk of developing PAD.
Occupations at Higher Risk for PAD
While PAD can affect individuals from various backgrounds, certain occupations may increase the risk due to specific job demands or environmental exposures:
- Sedentary Jobs: Professions that involve prolonged sitting or lack of physical activity, such as office workers, truck drivers, or call center employees, can contribute to the development of PAD.
- Manual Labor: Jobs that require prolonged standing or heavy physical exertion, such as construction workers, factory workers, or healthcare professionals, can put additional strain on the cardiovascular system and increase the risk of PAD.
- Exposure to Environmental Pollutants: Occupations that involve exposure to air pollution, chemicals, or other environmental toxins, such as mining, manufacturing, or certain industrial jobs, may increase the risk of PAD due to the damaging effects of these pollutants on the arteries.
It is essential for individuals in these professions to be aware of the potential risks and take proactive measures to maintain a healthy lifestyle, including regular exercise, a balanced diet, and routine medical check-ups.
Symptoms of Peripheral Arterial Disease
Many individuals with PAD may not experience any symptoms in the early stages of the disease. However, as the condition progresses and the arteries become more narrowed or blocked, symptoms may become more apparent. Common symptoms of PAD include:
- Claudication: This is the most common symptom of PAD, characterized by pain, cramping, or discomfort in the legs or buttocks that occurs during physical activity and subsides with rest.
- Numbness or Weakness: Reduced blood flow can cause numbness or weakness in the affected limb.
- Skin Changes: The skin on the affected limb may appear pale, shiny, or discolored due to poor circulation.
- Slow Healing Wounds: Wounds or sores on the affected limb may heal slowly or not at all due to inadequate blood supply.
- Coldness in the Limbs: The affected limb may feel cooler to the touch compared to other parts of the body.
- Erectile Dysfunction: PAD can also cause erectile dysfunction in men due to reduced blood flow.

It’s important to note that some individuals with PAD may not experience any symptoms, especially in the early stages of the disease. However, the presence of symptoms should prompt medical evaluation to determine the underlying cause and initiate appropriate treatment.
Diagnosis of Peripheral Arterial Disease
If PAD is suspected, healthcare professionals may perform various diagnostic tests to confirm the diagnosis and assess the severity of the condition. These tests may include:
-
Physical Examination: A healthcare provider may check for weak or absent pulses in the affected limb, as well as examine the skin for changes in color, temperature, or the presence of wounds.
-
Ankle-Brachial Index (ABI): This non-invasive test compares the blood pressure in the ankles with the blood pressure in the arms. A lower ankle pressure may indicate the presence of PAD.
-
Doppler Ultrasound: This imaging technique uses sound waves to evaluate blood flow in the arteries and detect any blockages or narrowing.
-
Angiography: In this invasive procedure, a contrast dye is injected into the arteries, and X-ray images are taken to visualize the blood vessels and identify any blockages or narrowing.
-
Magnetic Resonance Angiography (MRA) or Computed Tomography Angiography (CTA): These non-invasive imaging techniques can provide detailed images of the arteries and detect any blockages or narrowing.
By combining the results of these diagnostic tests, healthcare professionals can accurately diagnose PAD and determine the most appropriate course of treatment.
Treatment Options for Peripheral Arterial Disease
The treatment approach for PAD depends on the severity of the condition and the presence of any associated symptoms or complications. Treatment options may include:
-
Lifestyle Modifications:
- Smoking cessation
- Regular exercise and physical activity
- Maintaining a healthy diet
- Weight management
-
Medications:
- Antiplatelet medications (e.g., aspirin, clopidogrel) to prevent blood clots
- Cholesterol-lowering medications (e.g., statins) to reduce plaque buildup
- Blood pressure medications to control hypertension
- Medications to improve blood flow (e.g., cilostazol)
-
Revascularization Procedures:
- Angioplasty and stenting: A catheter is inserted into the blocked artery, and a balloon is inflated to open the blockage. A stent may be placed to keep the artery open.
- Bypass surgery: A healthy blood vessel is grafted to bypass the blocked artery, restoring blood flow to the affected limb.
-
Wound Care: For individuals with non-healing wounds or ulcers due to PAD, proper wound care and management are essential to prevent further complications.
-
Amputation: In severe cases where other treatments are ineffective, and the limb is severely compromised, amputation may be necessary to prevent the spread of infection or gangrene.
The treatment approach for PAD is tailored to each individual’s specific needs and may involve a combination of lifestyle modifications, medications, and revascularization procedures. Early diagnosis and treatment are crucial to prevent further progression of the disease and reduce the risk of complications.
Complications of Untreated Peripheral Arterial Disease
If left untreated, peripheral arterial disease can lead to severe and potentially life-threatening complications. Some of the most significant complications of untreated PAD include:
-
Critical Limb Ischemia: This condition occurs when the blockage in the arteries becomes so severe that it significantly reduces blood flow to the limbs, leading to tissue damage and potential gangrene. Critical limb ischemia can result in the need for amputation if not treated promptly.
-
Stroke: PAD is a risk factor for stroke, as the buildup of plaque in the arteries can also affect the blood vessels supplying the brain. Untreated PAD increases the likelihood of a stroke, which can lead to permanent neurological damage or even death.
-
Heart Attack: The atherosclerotic process that causes PAD can also affect the coronary arteries, increasing the risk of a heart attack or other cardiovascular events.
-
Impaired Wound Healing: Poor blood circulation due to PAD can impair the body’s ability to heal wounds, leading to chronic non-healing ulcers or infections that may require amputation.
-
Decreased Mobility and Quality of Life: As PAD progresses, the pain and discomfort associated with the condition can significantly limit mobility and physical activity, leading to a decreased quality of life.
It is crucial to seek medical attention and follow the recommended treatment plan if you have been diagnosed with PAD or are experiencing symptoms. Ignoring the condition or delaying treatment can have severe consequences and increase the risk of life-threatening complications.
Conclusion
Peripheral Arterial Disease is a serious condition that affects the arteries supplying blood to the limbs, primarily the legs. By understanding the causes, risk factors, symptoms, and available treatment options, individuals can take proactive steps to manage PAD effectively. Regular check-ups, lifestyle modifications, and adherence to prescribed treatments are essential for improving quality of life and preventing further complications associated with PAD.
For individuals in professions that may increase the risk of PAD, such as sedentary jobs, manual labor, or those exposed to environmental pollutants, it is crucial to be vigilant about maintaining a healthy lifestyle and seeking medical attention if any symptoms arise. Our Cypress, TX facility offers specialized care for patients with vascular conditions.

Remember, early detection and intervention are key in managing Peripheral Arterial Disease effectively. If you experience any symptoms or have risk factors for PAD, it is crucial to consult with our vascular specialists for proper evaluation and treatment. We also provide services in Houston, TX for your convenience. Ignoring the condition or delaying treatment can lead to severe and potentially life-threatening complications, including chronic venous insufficiency.
Want to keep up with your heart health?
Contact us to schedule an appointment.
