Chronic Venous Insufficiency
Varicose veins are a common vascular condition that affects millions of people worldwide. These abnormal, enlarged veins typically appear on the legs and feet, causing discomfort, pain, and cosmetic concerns for many individuals.
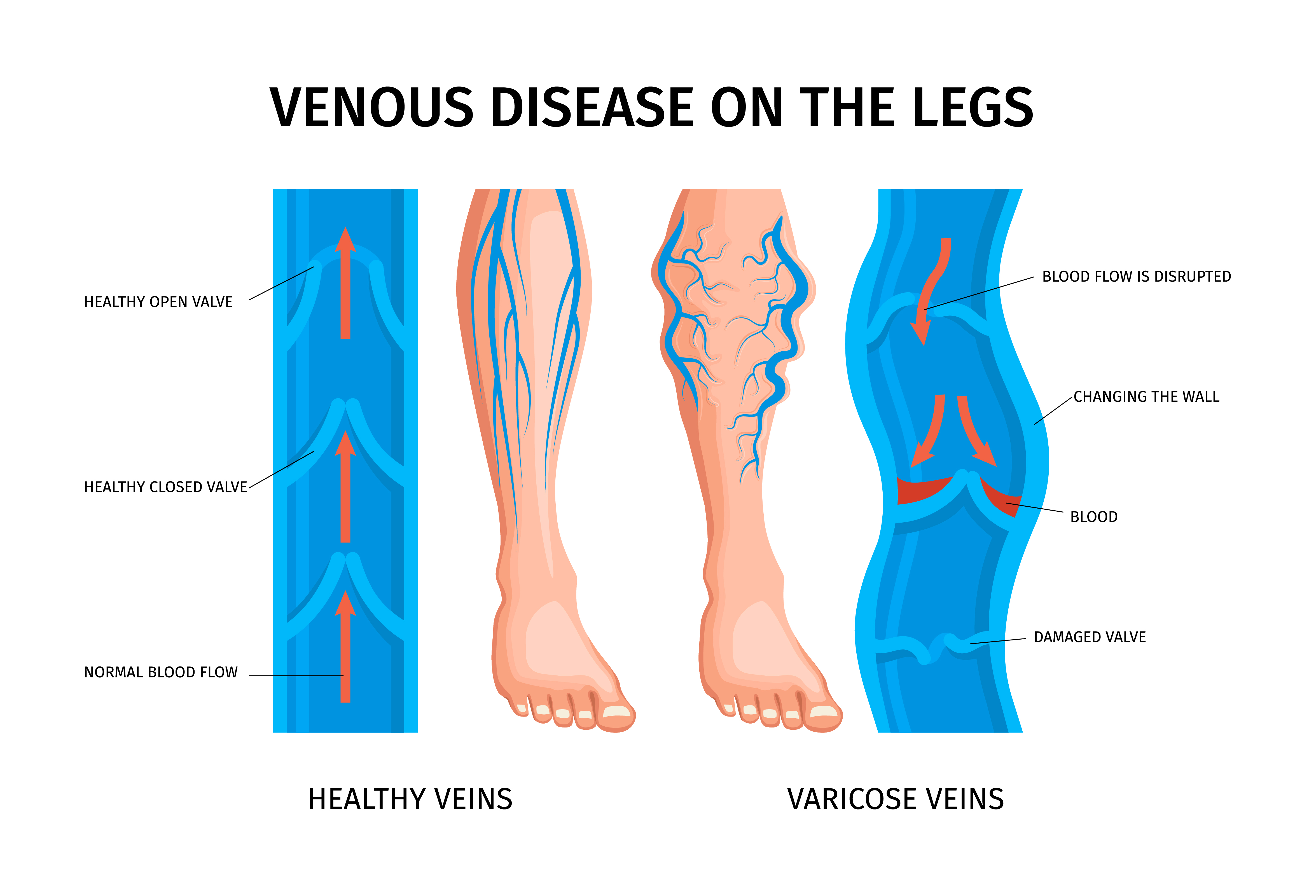
Table of Contents
Chronic Venous Insufficiency (CVI) - Understand Their Causes and Symptoms
What is Chronic Venous Insufficiency?
Chronic Venous Insufficiency (CVI) is a condition where the veins are unable to effectively circulate blood back to the heart, leading to chronic swelling and discomfort. This condition can affect anyone, regardless of age or health status.
CVI occurs when the valves in the leg veins that keep blood flowing toward the heart become weakened or damaged. This can cause blood to pool in the legs, leading to various symptoms such as leg swelling, pain, varicose veins, skin discoloration, and even ulcers.
The importance of addressing CVI lies in the fact that over 2.5 million individuals in the United States have this disorder, and around 20% present with venous ulcers as a complication. This can significantly reduce quality of life, lead to financial constraints, and cause disability. The estimated annual expenditures dedicated to the management of venous ulcer disease exceeds $1 billion.
Causes of Chronic Venous Insufficiency
CVI is often caused by:
-
Damage to vein valves: Valves in the veins can become damaged or weakened over time, making it difficult for blood to flow back up to the heart. This can be due to aging, prolonged standing or sitting, obesity, pregnancy, or a history of blood clots.
-
Increased pressure on the veins: Prolonged standing, sitting, or lying down can put additional pressure on the veins, leading to inflammation and swelling. Pregnancy and obesity also increase pressure on the leg veins.
-
Aging: As we age, our veins naturally lose their elasticity and become more prone to damage. The valves and muscles in the legs can weaken over time.
-
Genetic predisposition: Some people may be born with weaker vein valves or other genetic factors that increase their risk of developing CVI. Having a family history of varicose veins or venous insufficiency increases the risk.
Other risk factors include smoking, oral contraceptive use, hormone replacement therapy, sedentary lifestyle, and a history of leg injury or surgery.
Symptoms of Chronic Venous Insufficiency
Common symptoms of CVI include:
-
Chronic swelling: The affected area may become swollen and tender. Swelling often starts in the lower legs and ankles.
-
Discomfort or pain: You may experience a dull ache, heaviness, throbbing or itching in your legs, which worsens with standing and improves with rest and elevation. Pain can also manifest as leg fatigue, restless legs, or leg cramps.
-
Skin changes: Untreated CVI can lead to skin discoloration, thickening, dryness, itchiness, and ulceration. The skin may take on a leathery texture over time.
-
Varicose veins: Enlarged, twisted, rope-like superficial veins are a common sign of CVI. Spider veins, which look like red or purple sunbursts under the skin, may also appear.
What are the stages of CVI?
CVI progresses through several stages:
- Spider veins and reticular veins appear
- Varicose veins develop
- Swelling and skin changes occur
- Skin ulcers may form in advanced stages
A CVI diagnosis generally means that symptoms are at stage 3 or above. In the early stages, symptoms are generally mild. You may notice tired, achy legs or some spider veins. These early signs could get worse over time, so it's important to tell your doctor about them.
Chronic Vein Insufficiency Treatments
Treatment Options for chronic vein insufficiency
Fortunately, there are several treatment options available for CVI. These include:
-
Lifestyle changes: Regular exercise, maintaining a healthy weight, avoiding prolonged sitting or standing, elevating the legs, wearing loose clothing, and eating a balanced diet can all help promote healthy veins and reduce the risk of varicose veins. However, lifestyle changes alone are often not enough to fully manage CVI symptoms.
-
Compression therapy: Wearing compression stockings can help reduce swelling and alleviate pain. They provide graduated compression to promote blood flow. Prescription-strength garments fitted by a professional are recommended for anyone with venous disease.
-
Medications: Your doctor may prescribe antibiotics to treat infections or leg ulcers, or blood thinners to help prevent clots. Medicated wraps combining compression and topical medicines may also be used.
-
Minimally invasive procedures: Newer techniques allow doctors to treat problem veins with less invasive procedures:
-
Sclerotherapy involves injecting a chemical into affected veins to seal them closed. The body then redirects blood flow to healthier veins.
-
Radiofrequency ablation uses a thin catheter with a heated tip to seal off damaged veins from the inside.
-
VenaSeal applies medical adhesive inside dysfunctional veins to close them off.
-
Microphlebectomy removes troublesome veins through tiny 2-3mm incisions in the skin.
-
-
Surgery: In some cases, surgical removal (ligation) of the affected vein may be necessary. Surgical techniques aim to correct venous insufficiency by removing major sites of reflux. However, fewer than 1 in 10 people require surgery for CVI.
When Should I See My Healthcare Provider?
If you experience any symptoms of CVI, it's important to see your healthcare provider for an evaluation. Early diagnosis and treatment can help prevent complications.
You should also see your doctor if you have any risk factors for CVI, such as varicose veins, being over age 50, having a family history of vein problems, or a history of blood clots or leg injury. Your provider can assess your risk and help you take preventive measures.
What questions should I ask my healthcare provider?
- What is causing my CVI?
- What are my treatment options?
- How can I prevent CVI from worsening?
- Are there any lifestyle changes I should make?
- How often should I follow up with you about my condition?
Request an appointment
At Cypress Cardiovascular Institute, we understand the importance of addressing CVI in a timely and effective manner. Our experienced physicians and staff are dedicated to providing you with personalized care and treatment options tailored to your unique needs.
Don't let CVI disrupt your daily life. Contact us today to schedule an appointment and take the first step towards regaining your health and wellbeing!
- Varicose Veins
- Vein Disease
- Symptoms
Tommy Nguyen
Content Writer